Last updated: August 2020 | Time to read: 1 min 50 secs
Time to take action
World Bedwetting Day aims to encourage families to discuss bedwetting with their doctors and get the help they need.
This year, in this stressful lockdown situation, it is important to remember that bedwetting is a medical condition and talking to your doctor can help.
Get the facts
Bedwetting is common...but treatable
Your child may feel that wetting the bed is their fault, but it is not. Most children are dry at night by their fifth birthday. If your child is five years old and still wetting their bed, there may be a reason why.
With your help your child can understand the causes and what can be done about their bedwetting. There are treatments available, and your child’s doctor or nurse can explain how each treatment works and help choose the treatment that’s best for your child.
YOU’RE NOT ALONE...
More than 15% of children aged 7.5 years old wet the bed
In the UK half a million children aged 5–16 years old regularly wet the bed
Bedwetting can be distressing to your child and children who wet the bed have been shown to:

Have significantly lower self-esteem

Have the feeling of being 'different' to other children

Worry about others finding out
What is World bedwetting Day?
World Bedwetting Day began in 2015 by the International Children’s Continence Society (ICCS) and the European Society for Paediatric Urology (ESPU) to raise awareness about this common medical condition. This year’s theme focuses on ‘Time to Take Action’ as so much more can be done to diagnose and treat the condition.
By raising awareness of bedwetting as a common condition that can be treated, World Bedwetting Day aims to encourage families to discuss bedwetting with their doctor or nurse and get the help they need.
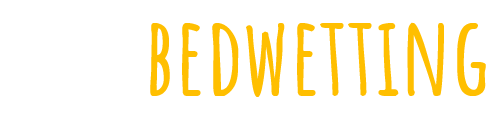
TOBY’S STORY...
Toby is like any typical 5-year-old – he loves to play and have fun with his friends. However, he would wet the bed at night which made him reluctant to go on sleep-overs at friends’ houses. Fortunately, his bedwetting was picked up at an early stage thanks to a helpful school nurse, GP and paediatric continence nurse.
Together they made sure he received the right treatment at the right time meaning his bedwetting was well managed and Toby was able to get back to socialising with his friends.
For more information visit:
http://www.paediatriccontinenceforum.org/wp-content/uploads/2017/07/PCF-Tobys-sub-optimal-versus-optimal-pathway-14th-March-2017.pdf
Subscribe to our newsletter
Enter your email address below
By clicking ‘subscribe’ you agree to be contacted by stopbedwetting.org via email newsletter. The newsletters will consist of updates relevant to bedwetting and will not offer recommendations on management options. Please see your doctor or nurse in this regard. For further information, please visit our privacy notice.
If you have specific questions or concerns, talk to your child's doctor, school nurse, health visitor or pharmacist.
Bladder and Bowel UK offer a confidential helpline. If you would like to speak to someone, email: bbuk@disabledliving.co.uk or phone: 0161 214 4591. You can also visit this website for more information: www.bbuk.org.uk/children-young-people/children-resources.
Support, information and resources are also available from ERIC, The Children’s Bowel and Bladder Charity: www.eric.org.uk and their freephone helpline: 0808 169 9949
This website is intended for UK residents only.
Job code: UK-MN-2300010 I Date of preparation: June 2023